 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Diabetic nephropathy

Diabetic nephropathy is a complication of diabetes that affects the kidneys. It is a type of kidney disease that occurs when high blood sugar levels in people with diabetes damage the blood vessels and filtering units (nephrons) in the kidneys. Over time, the kidneys may become less efficient at filtering waste products from the blood, leading to a buildup of toxins and water in the body.
The early stages of diabetic nephropathy often have no symptoms. As the condition progresses, symptoms may include swelling in the feet, ankles, or legs; fatigue; weakness; nausea; loss of appetite; and difficulty concentrating. If left untreated, diabetic nephropathy can lead to kidney failure, which may require dialysis or kidney transplant.
The diagnosis of diabetic nephropathy is usually based on a blood test to measure the level of a protein called albumin in the urine. If the albumin level is high, it may indicate that the kidneys are not functioning properly.
The treatment of diabetic nephropathy focuses on controlling blood sugar levels and blood pressure, as both can contribute to kidney damage. Medications that lower blood pressure, such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), are often prescribed to help slow the progression of diabetic nephropathy. In addition, a low-protein diet may be recommended to reduce the amount of waste products that the kidneys must filter.
Preventing diabetic nephropathy involves controlling blood sugar levels through proper diabetes management. This includes regular monitoring of blood sugar levels, taking diabetes medications as prescribed, following a healthy diet, and engaging in regular physical activity.
In conclusion, diabetic nephropathy is a serious complication of diabetes that can lead to kidney failure if left untreated. Early diagnosis and treatment are important to prevent the progression of the condition. By controlling blood sugar levels and blood pressure through proper diabetes management, you can help prevent diabetic nephropathy and other complications of diabetes. If you have diabetes, it is important to see your healthcare provider regularly to monitor your kidney function and overall health.
Research Papers
Disease Signs and Symptoms
- High blood pressure (hypertension)
- Itching
- Nausea or vomiting
- Loss of appetite
- Shortness of breath (dyspnea)
- Confusion (Hallucinations)
- Inability to hold urine
- Swollen arms or hands
- Swollen eye (Conjunctivitis)
- Excess protein or cloudy urine (proteinuria)
- Fatigue (Tiredness)
Disease Causes
Diabetic nephropathy
Diabetic nephropathy results when diabetes damages blood vessels and other cells in your kidneys.
How the kidneys work
Your kidneys contain millions of tiny blood vessel clusters (glomeruli) that filter waste from your blood. Severe damage to these blood vessels can lead to diabetic nephropathy, decreased kidney function and kidney failure.
Diabetic nephropathy causes
Diabetic nephropathy is a common complication of type 1 and type 2 diabetes.
Over time, poorly controlled diabetes can cause damage to blood vessel clusters in your kidneys that filter waste from your blood. This can lead to kidney damage and cause high blood pressure.
High blood pressure can cause further kidney damage by increasing the pressure in the delicate filtering system of the kidneys.
Disease Prevents
Diabetic nephropathy
To reduce your risk of developing diabetic nephropathy:
- Keep regular appointments for diabetes management. Keep annual appointments — or more-frequent appointments if recommended by your health care team — to monitor how well you are managing your diabetes and to screen for diabetic nephropathy and other complications.
- Treat your diabetes. With effective treatment of diabetes, you may prevent or delay diabetic nephropathy.
- Manage high blood pressure or other medical conditions. If you have high blood pressure or other conditions that increase your risk of kidney disease, work with your doctor to control them.
- Follow instructions on over-the-counter medications. Follow instructions on the packages of nonprescription pain relievers such as aspirin and nonsteroidal anti-inflammatory drugs, such as naproxen (Aleve) and ibuprofen (Advil, Motrin IB, others). For people with diabetic nephropathy, taking these types of pain relievers can lead to kidney damage.
- Maintain a healthy weight. If you're at a healthy weight, work to maintain it by being physically active most days of the week. If you need to lose weight, talk with your doctor about weight-loss strategies, such as increasing daily physical activity and consuming fewer calories.
- Don't smoke. Cigarette smoking can damage your kidneys and make existing kidney damage worse. If you're a smoker, talk to your doctor about strategies for quitting smoking. Support groups, counseling and some medications can all help you to stop.
Disease Treatments
The first step in treating diabetic nephropathy is to treat and control your diabetes and high blood pressure (hypertension). This includes diet, lifestyle changes, exercise and prescription medications. With good management of your blood sugar and hypertension, you may prevent or delay kidney dysfunction and other complications.
Medications
In the early stages of diabetic nephropathy, your treatment plan may include medications to manage the following:
- Blood pressure control. Medications called angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs) are used to treat high blood pressure.
- Blood sugar control. Medications can help control high blood sugar in people with diabetic nephropathy. Metformin (Fortamet, Glumetza, others) improves insulin sensitivity and lowers glucose production in the liver. Glucagon-like peptide 1 (GLP-1) receptor agonists help lower blood sugar levels by slowing digestion and stimulating insulin secretion in response to rising glucose levels. SGLT2 inhibitors limit the return of glucose to the bloodstream, leading to increased glucose excretion in the urine.
- High cholesterol. Cholesterol-lowering drugs called statins are used to treat high cholesterol and reduce protein in the urine.
- Kidney scarring. Finerenone (Kerendia) disrupts molecular activity believed to cause inflammation and tissue scarring in diabetic nephropathy. Research has shown that the drug may reduce the risk of kidney function decline, kidney failure, cardiovascular death, nonfatal heart attacks and hospitalization for heart failure in adults with chronic kidney disease associated with type 2 diabetes.
Your doctor will likely recommend follow-up testing at regular intervals to see whether your kidney disease remains stable or progresses.
Treatment for advanced diabetic nephropathy
Start Your Donor Evaluation
Begin the process of becoming a living kidney or liver donor by clicking here to complete a Health History Questionnaire.
If your disease progresses to kidney failure (end-stage kidney disease), your doctor will likely discuss options for care focused on either replacing the function of your kidneys or making you more comfortable. Options include:
- Kidney dialysis. This treatment removes waste products and extra fluid from your blood. The two main types of dialysis are hemodialysis and peritoneal dialysis. In the first, more common method, you may need to visit a dialysis center and be connected to an artificial kidney machine about three times a week, or you may have dialysis done at home by a trained caregiver. Each session takes 3 to 5 hours. The second method may be done at home as well.
- Transplant. In some situations, the best option is a kidney transplant or a kidney-pancreas transplant. If you and your doctor decide on transplantation, you'll be evaluated to determine whether you're eligible for this surgery.
- Symptom management. If you choose not to have dialysis or a kidney transplant, your life expectancy generally would be only a few months. You may receive treatment to help keep you comfortable.
Potential future treatments
In the future, people with diabetic nephropathy may benefit from treatments being developed using regenerative medicine. These techniques may help reverse or slow kidney damage caused by the disease. For example, some researchers think that if a person's diabetes can be cured by a future treatment such as pancreas islet cell transplant or stem cell therapy, kidney function may improve. These therapies, as well as new medications, are still under investigation.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Diabetic nephropathy and Learn More about Diseases

Primary lateral sclerosis (PLS)

Panic attacks and panic disorder

Anal itching

Hypothyroidism (underactive thyroid)
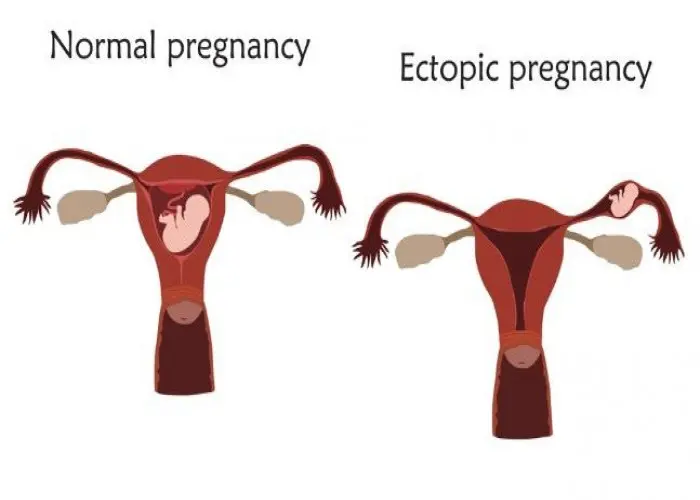
Ectopic pregnancy

Keratitis

Infertility (Sterility)
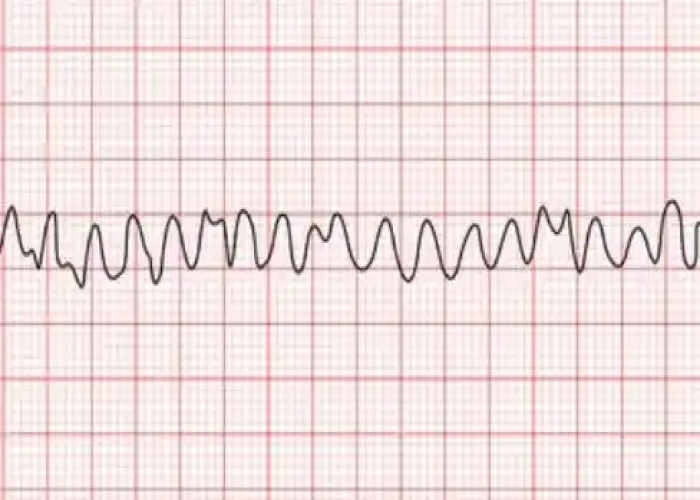
Ventricular fibrillation
diabetic nephropathy, ডায়াবেটিক নেফ্রোপ্যাথি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
