 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Chiari malformation

Chiari malformation is a structural abnormality in the brain in which the lower part of the cerebellum, known as the cerebellar tonsils, extend into the spinal canal. This can lead to symptoms such as headaches, neck pain, dizziness, balance problems, and in severe cases, paralysis. Treatment options may include observation, medications, or surgery depending on the severity and type of Chiari malformation.
Research Papers
Disease Signs and Symptoms
- Neck pain
- Weakness
- Ringing in ears (tinnitus)
- Dizziness (vertigo)
- Numbness or tingling in hands and feet
- Weakness and numbness in arms
- Numbness
- Poor coordination
- Tremor, lack of coordination or unsteady gait
- Slow heartbeat
Disease Causes
Chiari malformation
Chiari malformation type 1 occurs when the section of the skull containing a part of the brain (cerebellum) is too small or is deformed, thus putting pressure on and crowding the brain. The lower part of the cerebellum (tonsils) is displaced into the upper spinal canal.
Chiari malformation type 2 is nearly always associated with a form of spina bifida called myelomeningocele.
When the cerebellum is pushed into the upper spinal canal, it can interfere with the normal flow of cerebrospinal fluid that protects the brain and spinal cord.
This impaired circulation of cerebrospinal fluid can lead to the blockage of signals transmitted from the brain to the body, or to a buildup of spinal fluid in the brain or spinal cord.
Alternatively, the pressure from the cerebellum on the spinal cord or lower brainstem can cause neurological signs or symptoms.
Disease Prevents
Disease Treatments
Treatment for Chiari malformation depends on the severity and the characteristics of your condition.
If you have no symptoms, your doctor likely will recommend no treatment other than monitoring with regular examinations and MRIs.
When headaches or other types of pain are the primary symptom, your doctor may recommend pain medication.
Reducing pressure with surgery
Doctors usually treat symptomatic Chiari malformation with surgery. The goal is to stop the progression of changes in the anatomy of the brain and spinal canal, as well as ease or stabilize symptoms.
When successful, surgery can reduce pressure on the cerebellum and spinal cord and restore the normal flow of spinal fluid.
In the most common surgery for Chiari malformation, called posterior fossa decompression, the surgeon removes a small section of bone in the back of the skull, relieving pressure by giving the brain more room.
In many cases, the covering of the brain, called the dura mater, may be opened. Also, a patch may be sewn in place to enlarge the covering and provide more room for the brain. This patch may be an artificial material, or it could be tissue harvested from another part of the body.
Your doctor may also remove a small portion of the spinal column to relieve pressure on the spinal cord and allow more space for the spinal cord.
The surgical technique may vary, depending on whether a fluid-filled cavity (syrinx) is present, or if you have fluid in your brain (hydrocephalus). If you have a syrinx or hydrocephalus, you may need a tube (shunt) to drain the excess fluid.
Surgical risks and follow-up
Surgery involves risks, including the possibility of infection, fluid in the brain, cerebrospinal fluid leakage or problems with wound healing. Discuss the pros and cons with your doctor when deciding whether surgery is the most appropriate treatment for you.
The surgery reduces symptoms in most people, but if nerve injury in the spinal canal has already occurred, this procedure won't reverse the damage.
After the surgery, you'll need regular follow-up examinations with your doctor, including periodic imaging tests to assess the outcome of surgery and the flow of cerebrospinal fluid.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Chiari malformation and Learn More about Diseases
Premature ventricular contractions (PVCs)

Gaucher disease
Painful intercourse (dyspareunia)

Dyshidrosis

Trachoma
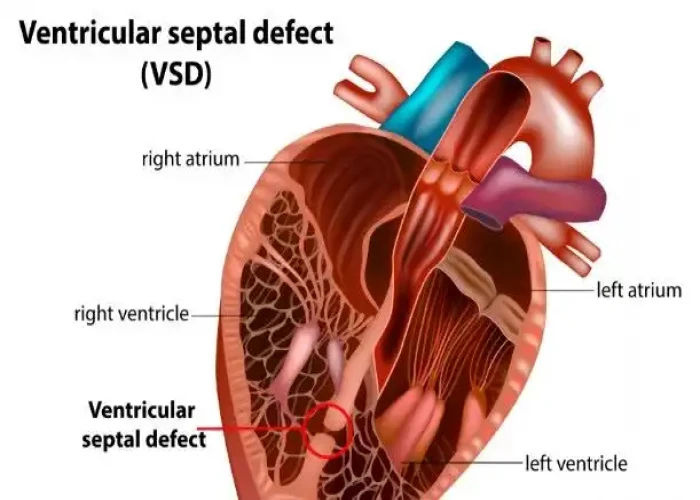
Ventricular septal defect (VSD)

Hirsutism
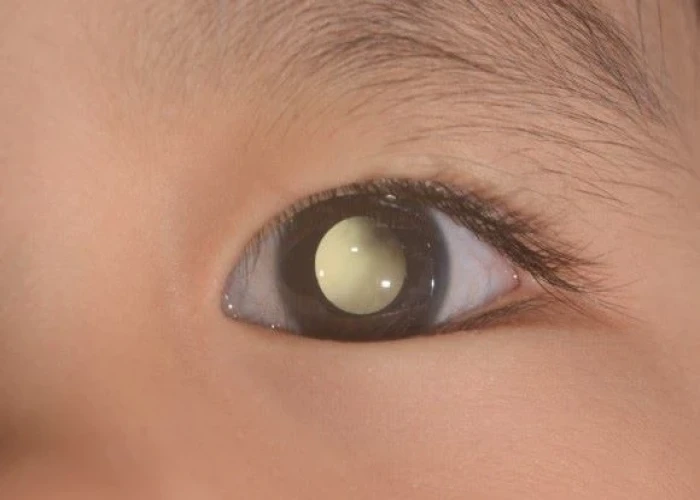
Retinoblastoma
Chiari malformation, Arnold chiari malformation, চিয়ারি বিকৃতি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
