 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Bronchiolitis
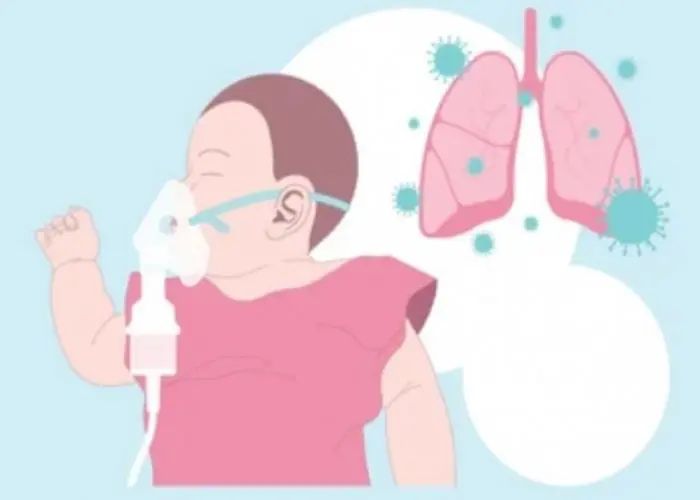
Bronchiolitis is a common respiratory infection that affects young children, particularly infants. It is usually caused by a viral infection that inflames and narrows the small airways in the lungs, making it difficult for the child to breathe. Symptoms of bronchiolitis may include cough, wheezing, rapid or shallow breathing, fever, and nasal congestion. The condition typically resolves on its own within a few weeks, but in some cases, hospitalization may be necessary for more severe cases. Treatment may include oxygen therapy, medications to relieve symptoms, and supportive care such as hydration and rest. Good hygiene practices such as frequent handwashing can help prevent the spread of the virus that causes bronchiolitis.
Research Papers
Disease Signs and Symptoms
- Runny nose
- Nose off
- Cough
- Fever
- Eating disorder
Disease Causes
Bronchiolitis
Bronchiolitis occurs when a virus infects the bronchioles, which are the smallest airways in your lungs. The infection makes the bronchioles swell and become inflamed. Mucus collects in these airways, which makes it difficult for air to flow freely in and out of the lungs.
Most cases of bronchiolitis are caused by the respiratory syncytial virus (RSV). RSV is a common virus that infects just about every child by 2 years of age. Outbreaks of RSV infection occur every winter, and individuals can be reinfected, as previous infection does not appear to cause lasting immunity. Bronchiolitis also can be caused by other viruses, including those that cause the flu or the common cold.
The viruses that cause bronchiolitis are easily spread. You can contract them through droplets in the air when someone who is sick coughs, sneezes or talks. You can also get them by touching shared objects — such as utensils, towels or toys — and then touching your eyes, nose or mouth.
Disease Prevents
Bronchiolitis
Because the viruses that cause bronchiolitis spread from person to person, one of the best ways to prevent it is to wash your hands frequently — especially before touching your baby when you have a cold or other respiratory illness. Wearing a face mask at this time is appropriate.
If your child has bronchiolitis, keep him or her at home until the illness is past to avoid spreading it to others.
Other commonsense ways to help curb infection include:
- Limit contact with people who have a fever or cold. If your child is a newborn, especially a premature newborn, avoid exposure to people with colds, especially in the first two months of life.
- Clean and disinfect surfaces. Clean and disinfect surfaces and objects that people frequently touch, such as toys and doorknobs. This is especially important if a family member is sick.
- Cover coughs and sneezes. Cover your mouth and nose with a tissue. Then throw away the tissue and wash your hands or use alcohol-based hand sanitizer.
- Use your own drinking glass. Don't share glasses with others, especially if someone in your family is ill.
- Wash hands often. Frequently wash your own hands and those of your child. Keep an alcohol-based hand sanitizer handy for yourself and your child when you're away from home.
- Breast-feed. Respiratory infections are significantly less common in breast-fed babies.
Vaccines and medications
There are no vaccines for the most common causes of bronchiolitis (RSV and rhinovirus). However, an annual flu shot is recommended for everyone older than 6 months.
Infants at high risk of the RSV infection, such as those born prematurely or with a heart or lung condition or who have a depressed immune system, may be given the medication palivizumab (Synagis) to decrease the likelihood of RSV infections.
Disease Treatments
Bronchiolitis typically lasts for two to three weeks. Most children with bronchiolitis can be cared for at home with supportive care. It's important to be alert for changes in breathing difficulty, such as struggling for each breath, being unable to speak or cry because of difficulty breathing, or making grunting noises with each breath.
Because viruses cause bronchiolitis, antibiotics — which are used to treat infections caused by bacteria — aren't effective against it. Bacterial infections such as pneumonia or an ear infection can occur along with bronchiolitis, and your doctor may prescribe an antibiotic for that infection.
Drugs that open the airways (bronchodilators) haven't been found to be routinely helpful and typically aren't given for bronchiolitis. In severe cases, your doctor may elect to try a nebulized albuterol treatment to see if it helps.
Oral corticosteroid medications and pounding on the chest to loosen mucus (chest physiotherapy) have not been shown to be effective treatments for bronchiolitis and are not recommended.
Disease Diagnoses
Disease Allopathic Generics
-
Ampicillin Sodium
1 vial orally or intravenously every 6 hours for 5 days.
-
Amoxicillin Trihydrate
1/2 vial orally or intravenously every 8 hours.
-
Cephalexin
1 250 mg or 500 mg or 1/2 spoon every 6 hours for 7-10 days.
-
Cephradine
Medicines containing cephradine can also be used in bronchiectasis.
1 capsule of 250 mg or 500 mg after 6 hours according to the severity of the disease.
-
Erythromycin (Oral)
Usually 1 tsp/ 1 pill (250mg) every 6 hours for 7-10 days. 1 of 500mg every 6 hours for 7-10 days in hard condition.
-
Ciprofloxacin
2 pills 500mg in the morning 500mg at night for 7-10 days in severe condition.
-
Pefloxacin Mesylate Dihydrate
1 pill in the morning 1 pill at night 7-10 days.
-
Cefuroxime Axetil
1+0+1 (7-10 days).
-
Levofloxacin Hemihydrate
250mg/500mg 1 daily.
-
Salbutamol
Medicines containing salubutamol as adjunctive therapy for respiratory distress.
1/2 pill 1/2 teaspoon 3 times a day.
-
Theophylline
1 pill or 1 spoon 3 times a day.
-
Dexamethasone
Bronchiectasis patients get good results if there are no contraindications to the use of cortisone group drugs, i.e. the patient does not have TB polyuria (diabetes) or hypertension (high blood pressure).
2 pills 3 times a day for 5 days, then 1 pill 3 times a day for 5 days and 1 pill 2 times a day for 5 days, finally 1/2 a pill 2 times a day for 5 days.
-
Chlorpheniramine Maleate
For cough.
Consume 2 spoons 2/3 times a day.
At the same time gargle 2/3 times a day with warm water mixed with salt which can be tolerated to reduce sore throat.
-
Paracetamol
For chest pain.
1 pill 3 times a day.
-
Ferrous Sulfate
For the patient's anemia.
Consume 1/2 teaspoon 3 times a day after meals.
-
Vitamin B complex
Vitamin B-complex medicines to increase strength if the patient feels very weak.
1 pill in the morning after food and 1 pill in the evening 3 times a day.
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Bronchiolitis and Learn More about Diseases

Bed-wetting
Brain metastases
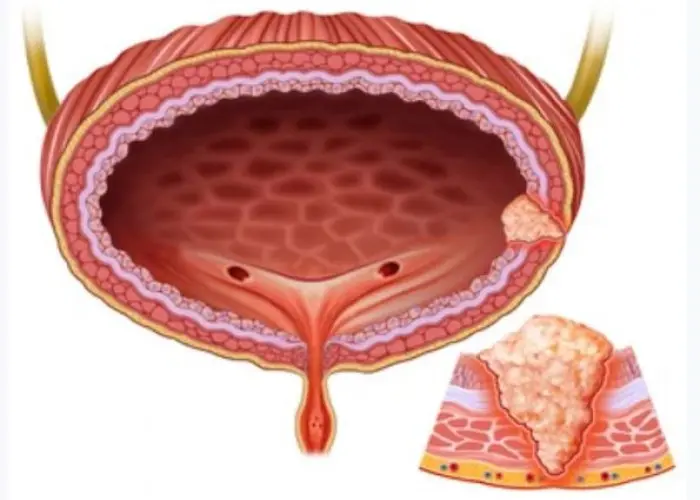
Bladder cancer

Guillain-Barre syndrome

Head and neck cancers
Sarcoma

Gingivitis
Delayed ejaculation
Bronchiolitis, Bronchiolitis treatment, Bronchiolar, ব্রঙ্কিওলাইটিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
