Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
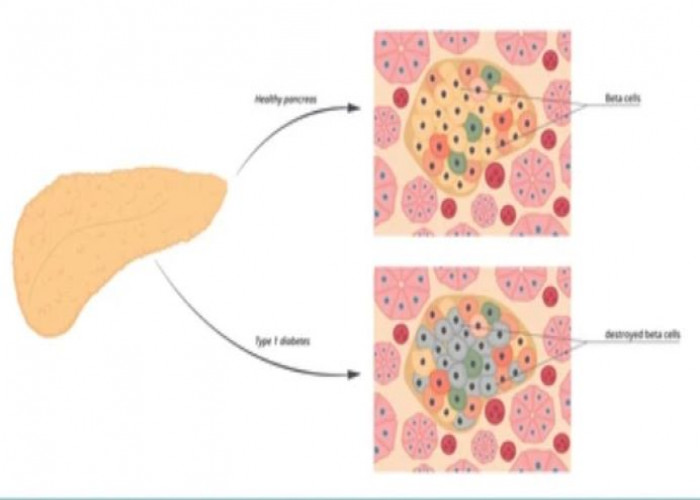
Autoimmune pancreatitis
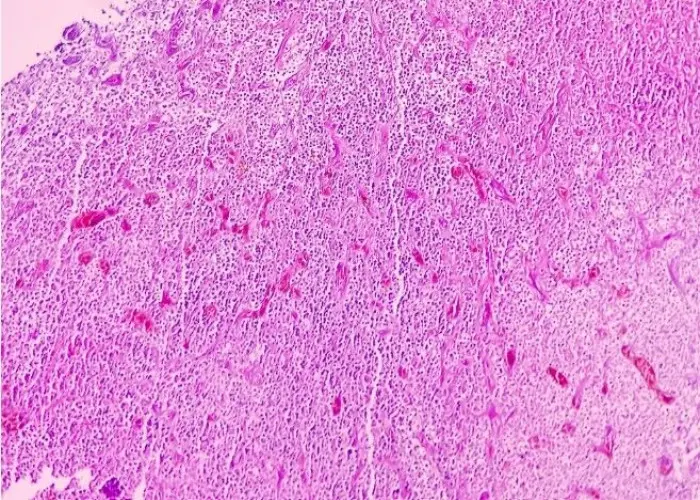
Autoimmune Pancreatitis (AIP) is a type of chronic pancreatitis that occurs when the immune system mistakenly attacks and inflames the pancreas, a gland located behind the stomach that helps produce digestive enzymes and regulate blood sugar levels through insulin production.
There are two types of autoimmune pancreatitis, known as type 1 and type 2. Type 1 is characterized by a benign course and is often associated with other autoimmune disorders, such as Sjogren's syndrome or IgG4-related disease. Type 2, on the other hand, is a more aggressive form that can cause significant destruction of the pancreas and other organs.
Symptoms of autoimmune pancreatitis may include abdominal pain, weight loss, jaundice, and elevated levels of pancreatic enzymes in the blood. Diagnosis may involve imaging studies such as an abdominal CT scan or MRI, as well as blood tests to check for elevated levels of certain antibodies.
Treatment of autoimmune pancreatitis typically involves a combination of immunosuppressive drugs and corticosteroids to reduce inflammation and prevent further damage to the pancreas. In severe cases, a pancreatectomy (surgery to remove part or all of the pancreas) may be necessary.
It's important to seek prompt medical attention if you suspect you may have autoimmune pancreatitis, as early diagnosis and treatment can help prevent complications and improve outcomes.
Research Papers
Disease Signs and Symptoms
- Dark urine color
- Pale stools or stools that float in the toilet
- Weight loss
- Loss of appetite
- Weakness
- Nausea or vomiting
- Abdomen pain
- Yellowing of skin and eyes (jaundice)
- Yellow skin
- Pale stool color
- Pain in your upper abdomen or middle part of your back
Disease Causes
Autoimmune pancreatitis
Doctors don't know what causes autoimmune pancreatitis, but as in other autoimmune diseases, it is thought to be caused by the body's immune system attacking healthy body tissue.
Disease Prevents
Disease Treatments
Biliary stenting. Before starting medication, sometimes doctors will insert a tube to drain the biliary ducts (biliary stenting) in people with symptoms of obstructive jaundice. Often, though, jaundice improves with steroid treatment alone. Sometimes drainage is recommended if the diagnosis is uncertain. Tissue samples and cells from the bile duct may be obtained at the time of stent placement.
Steroids. Symptoms of autoimmune pancreatitis often improve after a short course of prednisolone or prednisone. Many people respond quickly, even dramatically. Sometimes people get better without any treatment.
Immunosuppressants and immunomodulators. About 30% to 50% of the time in type 1 AIP and less than 10% of the time in type 2 AIP, the disease relapses, requiring additional treatment, sometimes long term.
To help reduce the serious side effects associated with extended steroid use, doctors often add drugs that suppress or modify the immune system, sometimes called steroid-sparing medications, to the treatment. You may be able to stop taking steroids altogether depending on your response to steroid-sparing medication.
Immunosuppressants and immunomodulators include mycophenolate (CellCept), mercaptopurine (Purinethol, Purixan), azathioprine (Imuran, Azasan) and rituximab (Rituxan). In general, they have been used in small sample groups and long-term benefits are still being studied.
Monitoring of other organ involvement. Type 1 AIP often is associated with other organ involvement, including enlarged lymph nodes and salivary glands, scarring of the bile ducts, liver inflammation, and kidney disease. Although these signs may lessen or disappear completely with steroid therapy, your doctor will continue to monitor you.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Autoimmune pancreatitis and Learn More about Diseases

Peanut allergy

Rheumatoid arthritis

Factor V Leiden

Menstrual cramps

Headaches in children
Buerger's disease

Nephrotic syndrome
Esthesioneuroblastoma
Autoimmune pancreatitis, Pancreas, অটোইমিউন অগ্ন্যাশয়
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.