Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
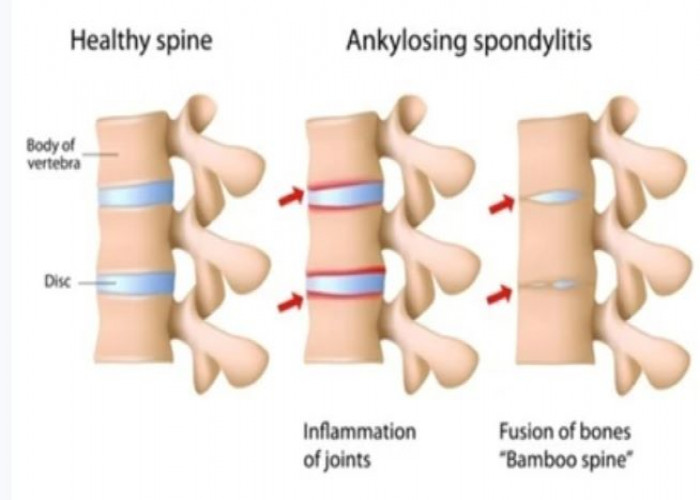
Ankylosing spondylitis
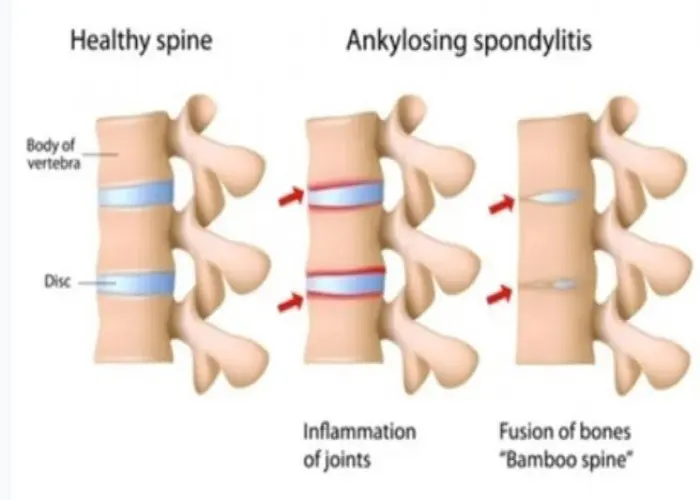
Ankylosing spondylitis is a type of arthritis that affects the spine and the joints between the spine and pelvis. It is a chronic condition that causes inflammation and pain in the spinal joints, leading to eventual fusion of the vertebrae and loss of mobility in the spine.
Ankylosing spondylitis is thought to be caused by a combination of genetic and environmental factors. It is more common in men and typically begins in early adulthood.
Symptoms of ankylosing spondylitis can include lower back pain and stiffness, especially in the morning or after periods of inactivity, fatigue, and loss of flexibility in the spine. In severe cases, the condition can cause a forward-stooped posture and difficulty breathing.
Treatment for ankylosing spondylitis can include nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and inflammation, physical therapy to maintain flexibility and strength, and disease-modifying antirheumatic drugs (DMARDs) to slow the progression of the disease.
If you have symptoms of ankylosing spondylitis or a family history of the condition, it's important to see a doctor for a diagnosis. Your doctor may perform tests such as a physical examination, X-rays, or an MRI to diagnose ankylosing spondylitis and determine the best course of treatment.
Research Papers
Disease Signs and Symptoms
- Neck pain
- Spine and pelvis pain
- The affected places are the cartilage between your breastbone and ribs
Disease Causes
Ankylosing spondylitis
Ankylosing spondylitis has no known specific cause, though genetic factors seem to be involved. In particular, people who have a gene called HLA-B27 are at a greatly increased risk of developing ankylosing spondylitis. However, only some people with the gene develop the condition.
Disease Prevents
Disease Treatments
The goal of treatment is to relieve pain and stiffness and prevent or delay complications and spinal deformity. Ankylosing spondylitis treatment is most successful before the disease causes irreversible damage.
The goal of treatment is to relieve pain and stiffness and prevent or delay complications and spinal deformity. Ankylosing spondylitis treatment is most successful before the disease causes irreversible damage.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) — such as naproxen (Aleve, Naprosyn, others) and ibuprofen (Advil, Motrin IB, others) — are the medications doctors most commonly use to treat ankylosing spondylitis. These medications can relieve inflammation, pain and stiffness, but they also might cause gastrointestinal bleeding.
If NSAIDs aren't helpful, your doctor might suggest starting a tumor necrosis factor (TNF) blocker or an interleukin-17 (IL-17) inhibitor. These drugs are injected under the skin or through an intravenous line. These types of medications can reactivate untreated tuberculosis and make you more prone to infections.
Examples of TNF blockers include:
- Adalimumab (Humira)
- Certolizumab pegol (Cimzia)
- Etanercept (Enbrel)
- Golimumab (Simponi)
- Infliximab (Remicade)
IL-17 inhibitors used to treat ankylosing spondylitis include secukinumab (Cosentyx) and ixekizumab (Taltz).
Therapy
Physical therapy is an important part of treatment and can provide a number of benefits, from pain relief to improved strength and flexibility. A physical therapist can design specific exercises for your needs. To help preserve good posture, you may be taught:
- Range-of-motion and stretching exercises
- Strengthening exercises for abdominal and back muscles
- Proper sleeping and walking positions
Surgery
Most people with ankylosing spondylitis don't need surgery. Surgery may be recommended if you have severe pain or if a hip joint is so damaged that it needs to be replaced.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Ankylosing spondylitis and Learn More about Diseases

Typhoid fever

Angina

Pruritus Vulva

Progeria
Frontotemporal dementia

Hypospadias

Plantar warts

Peyronie's disease
Ankylosing spondylitis, Ankylosing spondylitis treatment, Spondylitis ankylosans, অ্যাঙ্কিলোসিং স্পনডিলাইটিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.