 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Stress incontinence

Stress incontinence is a type of urinary incontinence that is caused by pressure or stress on the bladder, leading to the unintentional leakage of urine. This pressure may be caused by activities such as coughing, sneezing, laughing, lifting, or exercising.
Stress incontinence is most common in women, particularly after pregnancy and childbirth, as well as in older women and men who have had prostate surgery. The symptoms of stress incontinence may include:
- Leakage of urine during activities that put pressure on the bladder
- A feeling of urgency to urinate
- Frequent urination, including during the night
- Difficulty emptying the bladder completely
There are several treatment options for stress incontinence, including:
- Lifestyle changes: Lifestyle changes can help reduce symptoms of stress incontinence. These may include losing weight, quitting smoking, avoiding alcohol and caffeine, and practicing pelvic floor exercises.
- Medications: Certain medications, such as alpha-adrenergic agonists and anticholinergics, may be prescribed to treat stress incontinence.
- Medical devices: Medical devices, such as a pessary, may be recommended to help support the bladder and prevent leakage.
- Surgery: Surgery may be recommended for severe cases of stress incontinence that have not responded to other treatments. Surgical options may include bladder suspension surgery, sling procedures, or artificial urinary sphincter implants.
It is important to talk to a healthcare provider if you are experiencing symptoms of stress incontinence, as there are many effective treatments available.
Research Papers
Disease Signs and Symptoms
- Cough
- Sneeze
- Inability to hold urine
- Bladder problems
- Loss of bowel or bladder function
Disease Causes
Stress incontinence
Stress incontinence occurs when the muscles and other tissues that support the urethra (pelvic floor muscles) and the muscles that control the release of urine (urinary sphincter) weaken.
The bladder expands as it fills with urine. Typically, valve-like muscles in the urethra — the short tube that carries urine out of your body — stay closed as the bladder expands, preventing urine leakage until you reach a bathroom. But when those muscles weaken, anything that exerts force on the abdominal and pelvic muscles — sneezing, bending over, lifting or laughing hard, for instance — can put pressure on your bladder and cause urine leakage.
Your pelvic floor muscles and urinary sphincter may lose strength because of:
- Childbirth. In women, tissue or nerve damage during delivery of a child can weaken the pelvic floor muscles or the sphincter. Stress incontinence from this damage may begin soon after delivery or occur years later.
- Prostate surgery. In men, the surgical removal of the prostate gland to treat prostate cancer (prostatectomy) is the most common factor leading to stress incontinence. This procedure can weaken the sphincter, which lies directly below the prostate gland and encircles the urethra.
Contributing factors
Other factors that may worsen stress incontinence include:
- Illnesses that cause chronic coughing
- Obesity
- Smoking, which can cause frequent coughing
- High-impact activities, such as running and jumping, over many years
Disease Prevents
Disease Treatments
Your health care provider may recommend a combination of strategies to treat incontinence. If an underlying cause or contributing factor, such as a urinary tract infection, is identified, you'll also receive treatment for the condition.
Behavior therapies
Behavior therapies may help you eliminate or lessen episodes of stress incontinence. The treatments your doctor recommends may include:
- Pelvic floor muscle exercises. Your provider or physical therapist can help you learn how to do Kegel exercises to strengthen your pelvic floor muscles and urinary sphincter. Just like any other exercise routine, how well Kegel exercises work for you depends on whether you perform them regularly.
- A technique called biofeedback can be used along with Kegel exercises to make them more effective. Biofeedback involves the use of pressure sensors or electrical stimulation to reinforce the proper muscle contractions.
- Fluid consumption. Your provider may recommend how much and when you should consume fluids during the day and evening. However, don't limit what you drink so much that you become dehydrated.
- Your provider may also suggest that you avoid caffeinated, carbonated and alcoholic beverages, which may irritate and affect bladder function in some people. If you find that using fluid schedules and avoiding certain beverages significantly improve leakage, you'll have to decide whether making these changes in your diet are worth it.
- Healthy lifestyle changes. Quitting smoking, losing excess weight or treating a chronic cough will lessen your risk of stress incontinence and improve your symptoms.
- Bladder training. Your provider might recommend a schedule for toileting if you have mixed incontinence. More frequent voiding of the bladder may reduce the number or severity of urge incontinence episodes.
Medications
There are no approved medications to specifically treat stress incontinence in the United States. The antidepressant duloxetine (Cymbalta, Drizalma Sprinkle) is used for the treatment of stress incontinence in Europe, however.
Symptoms quickly return when the drug is stopped. Nausea is the most common side effect that makes people stop taking the medication.
Devices
Certain devices designed for women may help control stress incontinence, including:
- Vaginal pessary. A specialized urinary incontinence pessary, shaped like a ring with two bumps that sit on each side of the urethra, is fitted and put into place by your provider. It helps support your bladder base to prevent urine leakage during activity, especially if your bladder has dropped (prolapsed).
- This is a good choice if you wish to avoid surgery. A pessary will require routine removal and cleaning. Pessaries are used mostly in people who also have pelvic organ prolapse.
- Urethral inserts. This small tampon-like disposable device inserted into the urethra acts as a barrier to prevent leakage. It's usually used to prevent incontinence during a specific activity, but it may be worn throughout the day.
- Urethral inserts can be worn for up to eight hours a day. Urethral inserts are generally used only for heavy activity, such as repeated lifting, running or playing tennis.
Surgery
Surgical interventions to treat stress incontinence are designed to improve closure of the sphincter or support the bladder neck. Surgical options include:
- Sling procedure. This is the most common procedure performed in women with stress urinary incontinence. In this procedure, the surgeon uses the person's own tissue, synthetic material (mesh), or animal or donor tissue to create a sling or hammock that supports the urethra.
- Slings are also used for men with mild stress incontinence. The technique may ease symptoms of stress incontinence in some men.
- Injectable bulking agents. Synthetic polysaccharides or gels may be injected into tissues around the upper portion of the urethra. These materials bulk up the area around the urethra, improving the closing ability of the sphincter.
- Retropubic colposuspension. This surgical procedure uses sutures attached to ligaments along the pubic bone to lift and support tissues near the bladder neck and upper portion of the urethra. This surgery can be done laparoscopically or by an incision in the abdomen.
- Inflatable artificial sphincter. This surgically implanted device is used to treat men. A cuff, which fits around the upper portion of the urethra, replaces the function of the sphincter. Tubes connect the cuff to a pressure-regulating balloon in the pelvic region and a manually operated pump in the scrotum.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Stress incontinence and Learn More about Diseases
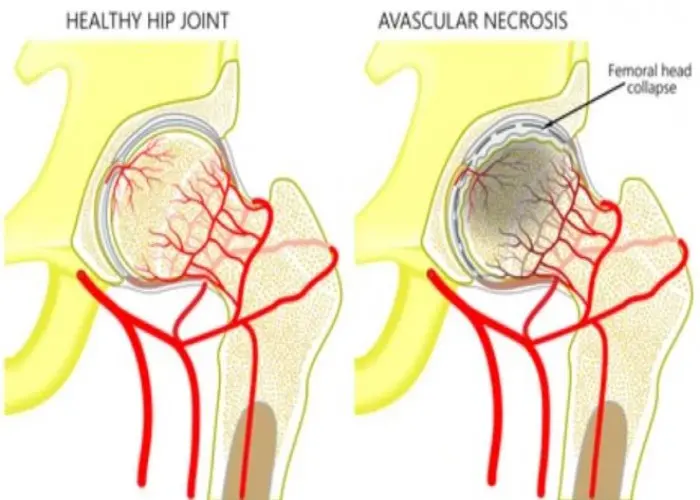
Avascular necrosis
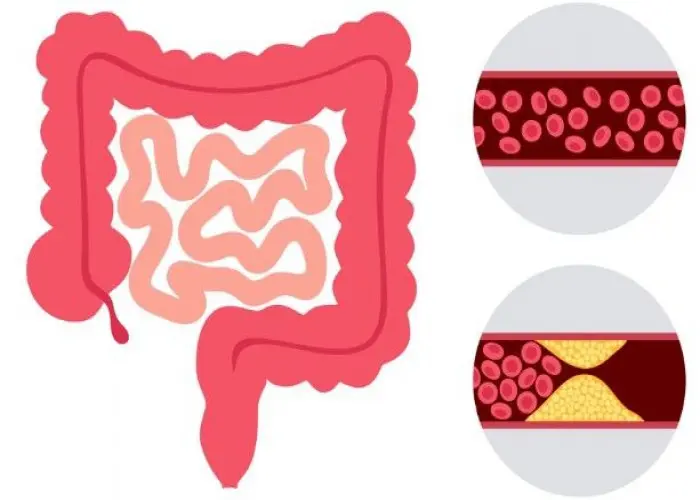
Ischemic colitis

Athlete's foot
Salivary gland tumors
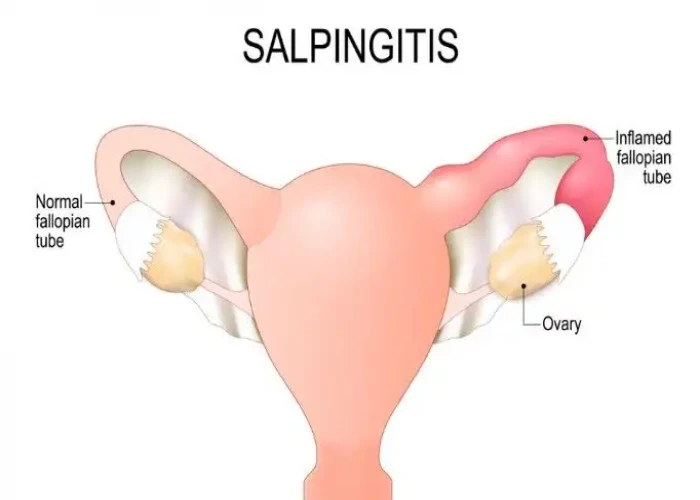
Salpingitis

Chemo brain
Sleep terrors (night terrors)

Kidney stones
Stress incontinence, স্ট্রেস ইনকন্টিনেন্স
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
