 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Rectal cancer

Rectal cancer is a type of cancer that develops in the rectum, which is the last several inches of the large intestine, located just above the anus. Like other types of cancer, rectal cancer occurs when abnormal cells in the rectum grow and multiply uncontrollably, forming a tumor.
The exact cause of rectal cancer is not known, but risk factors include age, family history of colon or rectal cancer, a personal history of colon or rectal polyps, a diet high in red or processed meats, and inflammatory bowel disease.
Symptoms of rectal cancer can include changes in bowel habits, such as diarrhea, constipation, or narrow stools, blood in the stool, abdominal discomfort or pain, and unintended weight loss. However, in some cases, rectal cancer may not cause any noticeable symptoms.
Treatment for rectal cancer typically involves surgery to remove the cancerous tissue, followed by radiation therapy and/or chemotherapy to destroy any remaining cancer cells. The specific treatment plan will depend on the stage and location of cancer, as well as the individual's overall health and other factors.
Prevention of rectal cancer includes making lifestyle changes to reduce risk factors, such as adopting a healthy diet rich in fruits, vegetables, and whole grains, getting regular exercise, maintaining a healthy weight, and quitting smoking. It is also important to undergo regular screening tests, such as colonoscopy, to detect any signs of colon or rectal cancer in their early stages when they are most treatable.
If you experience any symptoms of rectal cancer, or if you have risk factors for the condition, it is important to talk to your healthcare provider to determine the appropriate screening and prevention measures for you.
Research Papers
Disease Signs and Symptoms
- Bowel incontinence
- Blood in stool
- Abdomen pain
- Weight loss
- Weakness
- Fatigue (Tiredness)
- A change in bowel habits, such as diarrhea, constipation or more-frequent bowel movements
Disease Causes
Rectal cancer
Rectal cancer begins when healthy cells in the rectum develop changes (mutations) in their DNA. A cell's DNA contains the instructions that tell a cell what to do.
The changes tell the cells to grow uncontrollably and to continue living after healthy cells would die. The accumulating cells can form a tumor. With time, the cancer cells can grow to invade and destroy healthy tissue nearby. And cancerous cells can break away and travel (metastasize) to other parts of the body.
For most rectal cancers, it's not clear what causes the mutations that cause the cancer to form.
Inherited gene mutations that increase the risk of colon and rectal cancer
In some families, gene mutations passed from parents to children increase the risk of colorectal cancer. These mutations are involved in only a small percentage of rectal cancers. Some genes linked to colorectal cancer increase the risk of developing the disease, but they don't make it inevitable.
Two well-defined genetic colorectal cancer syndromes are:
- Lynch syndrome. Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), increases the risk of colon cancer and other cancers. People with Lynch syndrome tend to develop colon cancer before age 50.
- Familial adenomatous polyposis (FAP). FAP is a rare disorder that causes thousands of polyps in the lining of your colon and rectum. People with untreated FAP have a significantly increased risk of developing colon or rectal cancer before age 40.
Genetic testing can detect these and other, rarer inherited colorectal cancer syndromes. If you're concerned about your family history of colon cancer, talk to your doctor about whether your family history suggests you have a risk of these conditions.
Disease Prevents
Rectal cancer
To reduce your risk of colorectal cancer, consider trying to:
- Talk to your doctor about cancer screening. Colorectal cancer screening reduces the risk of cancer by identifying precancerous polyps in the colon and rectum that could develop into cancer. Ask your doctor when you should begin screening. Most medical organizations recommend starting screening around age 50, or earlier if you have risk factors for colorectal cancer.
- Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you.
- Exercise most days of the week. Try to get at least 30 minutes of exercise on most days. If you've been inactive, start slowly and build up gradually to 30 minutes. Also, talk to your doctor before beginning any exercise program.
- Eat a variety of fruits, vegetables and whole grains. Fruits, vegetables and whole grains contain vitamins, minerals, fiber and antioxidants, which may play a role in cancer prevention. Choose a variety of fruits and vegetables so that you get an array of vitamins and nutrients.
- Maintain a healthy weight. If you're at a healthy weight, maintain it by exercising regularly and choosing a healthy diet. If you're overweight, work to lose weight slowly by increasing exercise and reducing the number of calories you eat.
- Stop smoking. If you smoke, stop. If you're having trouble quitting, talk to your doctor about options. Medications and counseling may help.
- Drink alcohol in moderation, if at all. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
Disease Treatments
Rectal cancer treatment often involves a combination of therapies. When possible, surgery is used to cut away the cancer cells. Other treatments, such as chemotherapy and radiation therapy, may be used after surgery to kill any cancer cells that remain and reduce the risk that cancer will return.
If surgeons are concerned that the cancer can't be removed completely without hurting nearby organs and structures, your doctor may recommend a combination of chemotherapy and radiation therapy as your initial treatment. These combined treatments may shrink the cancer and make it easier to remove during an operation.
Surgery
Rectal cancer is often treated with surgery to remove the cancer cells. Which operation is best for you depends on your particular situation, such as the location and stage of your cancer, how aggressive the cancer cells are, your overall health, and your preferences.
Operations used to treat rectal cancer include:
- Removing very small cancers from the inside of the rectum. Very small rectal cancers may be removed using a colonoscope or another specialized type of scope inserted through the anus (transanal local excision). Surgical tools can be passed through the scope to cut away the cancer and some of the healthy tissue around it.
- This procedure might be an option if your cancer is small and unlikely to spread to nearby lymph nodes. If a lab analysis finds that your cancer cells are aggressive or more likely to spread to the lymph nodes, your doctor may recommend additional surgery.
- Removing all or part of the rectum. Larger rectal cancers that are far enough away from the anal canal might be removed in a procedure (low anterior resection) that removes all or part of the rectum. Nearby tissue and lymph nodes are also removed. This procedure preserves the anus so that waste can leave the body normally.
- How the procedure is performed depends on the cancer's location. If cancer affects the upper portion of the rectum, that part of the rectum is removed and then the colon is attached to the remaining rectum (colorectal anastomosis). All of the rectum may be removed if the cancer is located in the lower portion of the rectum. Then the colon is shaped into a pouch and attached to the anus (coloanal anastomosis).
- Removing the rectum and anus. For rectal cancers that are located near the anus, it might not be possible to remove the cancer completely without damaging the muscles that control bowel movements. In these situations, surgeons may recommend an operation called abdominoperineal resection (APR) to remove the rectum, anus and some of the colon, as well as nearby tissue and lymph nodes.
- The surgeon creates an opening in the abdomen and attaches the remaining colon (colostomy). Waste leaves your body through the opening and collects in a bag that attaches to your abdomen.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells. For rectal cancer, chemotherapy might be recommended after surgery to kill any cancer cells that might remain.
Chemotherapy combined with radiation therapy might also be used before an operation to shrink a large cancer so that it's easier to remove with surgery.
Chemotherapy can also be used to relieve symptoms of rectal cancer that can't be removed with surgery or that has spread to other areas of the body.
Radiation therapy
Radiation therapy uses powerful energy sources, such as X-rays and protons, to kill cancer cells. In people with rectal cancer, radiation therapy is often combined with chemotherapy that makes the cancer cells more likely to be damaged by the radiation. It can be used after surgery to kill any cancer cells that might remain. Or it can be used before surgery to shrink a cancer and make it easier to remove.
When surgery isn't an option, radiation therapy might be used to relieve symptoms, such as pain.
Combined chemotherapy and radiation therapy
Combining chemotherapy and radiation therapy (chemoradiotherapy) makes cancer cells more vulnerable to radiation. The combination is often used for larger rectal cancers and those that have a higher risk of returning after surgery.
Chemoradiotherapy may be recommended:
- Before surgery. Chemoradiotherapy may help shrink the cancer enough to make a less invasive surgery possible. The combined treatment may increase the chance that your operation will leave the anal area intact so waste can leave the body normally after surgery.
- After surgery. If surgery was your first treatment, your doctor may recommend chemoradiotherapy afterward if there's an increased risk that your cancer may return.
- As the primary treatment. Your doctor may recommend chemoradiotherapy to control the growth of cancer if your rectal cancer is advanced or if surgery isn't an option.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die.
Targeted drugs are usually combined with chemotherapy. Targeted drugs are typically reserved for people with advanced rectal cancer.
Immunotherapy
Immunotherapy is a drug treatment that uses your immune system to fight cancer. Your body's disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy is usually reserved for advanced rectal cancer.
Supportive (palliative) care
Palliative care is focused on providing relief from pain and other symptoms of a severe illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Rectal cancer and Learn More about Diseases
Viral hemorrhagic fevers
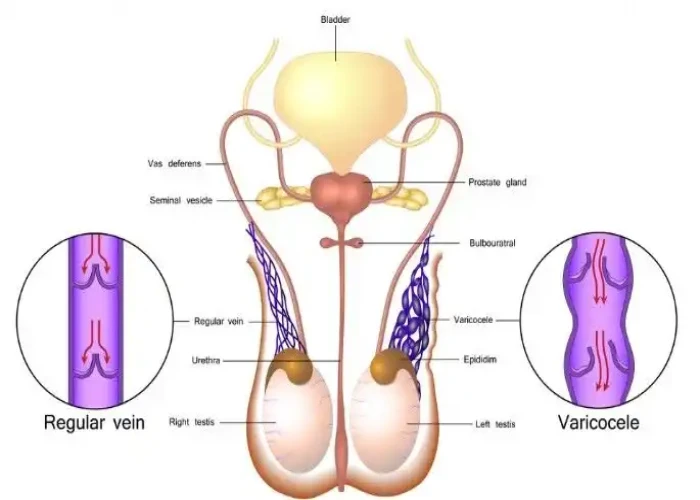
Varicocele

Urinary incontinence
Sarcoma

Brain AVM (arteriovenous malformation)

Reactive arthritis

Albinism

Cold sore
rectal cancer, মলদ্বারে ক্যান্সার
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
