 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Obsessive-compulsive disorder (OCD)

Obsessive-compulsive disorder (OCD) is a mental health disorder characterized by the presence of obsessions and/or compulsions that are difficult to control and cause significant distress or impairment in daily functioning.
Obsessions are recurrent, intrusive, and unwanted thoughts, images, or urges that are experienced as distressing or anxiety-provoking. Common themes of obsessions include contamination, harm, or symmetry. Compulsions are repetitive behaviors or mental acts that are performed to reduce anxiety or prevent a feared outcome. Common compulsions include cleaning, checking, counting, or repeating words or phrases.
The diagnosis of OCD is based on the presence of obsessions and/or compulsions that consume significant time or interfere with daily life, cause significant distress or anxiety, and are not attributable to another medical or psychiatric condition. OCD can co-occur with other mental health disorders, such as depression, anxiety disorders, or tic disorders.
The causes of OCD are not fully understood, but it is believed to involve a combination of genetic, environmental, and neurobiological factors. Treatment for OCD typically involves cognitive-behavioral therapy (CBT), which focuses on exposing the person to the feared stimuli and helping them to develop more adaptive responses to the anxiety-provoking thoughts or situations. Medications, such as selective serotonin reuptake inhibitors (SSRIs), may also be helpful in reducing the symptoms of OCD.
With treatment, many people with OCD are able to manage their symptoms and improve their quality of life. However, OCD is a chronic condition that can be difficult to fully cure. People with OCD may experience periods of remission and relapse over time, and ongoing treatment may be necessary to maintain symptom control.
Research Papers
Disease Signs and Symptoms
- Doubting and having difficulty tolerating uncertainty
- Silently repeating a prayer, word or phrase
- Checking the stove repeatedly to make sure it's off
- Checking doors repeatedly to make sure they're locked
- Avoidance of situations that can trigger obsessions, such as shaking hands
- Thoughts about shouting obscenities or acting inappropriately in public
- Images of driving the car into a crowd of people
- Intense stress when objects aren't orderly or facing a certain way
- Doubts that locked the door or turned off the stove
- Fear of being contaminated by touching objects others have touched
- Aggressive or horrific thoughts about losing control and harming or others
- Needing things orderly and symmetrical
- Unwanted thoughts and fears (obsessions)
Disease Causes
Obsessive-compulsive disorder (OCD)
The cause of obsessive-compulsive disorder isn't fully understood. Main theories include:
- Biology. OCD may be a result of changes in your body's own natural chemistry or brain functions.
- Genetics. OCD may have a genetic component, but specific genes have yet to be identified.
- Learning. Obsessive fears and compulsive behaviors can be learned from watching family members or gradually learned over time.
Disease Prevents
Obsessive-compulsive disorder (OCD)
There's no sure way to prevent obsessive-compulsive disorder. However, getting treatment as soon as possible may help prevent OCD from worsening and disrupting activities and your daily routine.
Disease Treatments
Obsessive-compulsive disorder treatment may not result in a cure, but it can help bring symptoms under control so that they don't rule your daily life. Depending on the severity of OCD, some people may need long-term, ongoing or more intensive treatment.
The two main treatments for OCD are psychotherapy and medications. Often, treatment is most effective with a combination of these.
Psychotherapy
Cognitive behavioral therapy (CBT), a type of psychotherapy, is effective for many people with OCD. Exposure and response prevention (ERP), a component of CBT therapy, involves gradually exposing you to a feared object or obsession, such as dirt, and having you learn ways to resist the urge to do your compulsive rituals. ERP takes effort and practice, but you may enjoy a better quality of life once you learn to manage your obsessions and compulsions.
Medications
Certain psychiatric medications can help control the obsessions and compulsions of OCD. Most commonly, antidepressants are tried first.
Antidepressants approved by the U.S. Food and Drug Administration (FDA) to treat OCD include:
- Clomipramine (Anafranil) for adults and children 10 years and older
- Fluoxetine (Prozac) for adults and children 7 years and older
- Fluvoxamine for adults and children 8 years and older
- Paroxetine (Paxil, Pexeva) for adults only
- Sertraline (Zoloft) for adults and children 6 years and older
However, your doctor may prescribe other antidepressants and psychiatric medications.
Medications: What to consider
Here are some issues to discuss with your doctor about medications for OCD:
- Choosing a medication. In general, the goal is to effectively control symptoms at the lowest possible dosage. It's not unusual to try several drugs before finding one that works well. Your doctor might recommend more than one medication to effectively manage your symptoms. It can take weeks to months after starting a medication to notice an improvement in symptoms.
- Side effects. All psychiatric medications have potential side effects. Talk to your doctor about possible side effects and about any health monitoring needed while taking psychiatric drugs. And let your doctor know if you experience troubling side effects.
- Suicide risk. Most antidepressants are generally safe, but the FDA requires that all antidepressants carry black box warnings, the strictest warnings for prescriptions. In some cases, children, teenagers and young adults under 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. If suicidal thoughts occur, immediately contact your doctor or get emergency help. Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
- Interactions with other substances. When taking an antidepressant, tell your doctor about any other prescription or over-the-counter medications, herbs or other supplements you take. Some antidepressants can make some other medications less effective and cause dangerous reactions when combined with certain medications or herbal supplements.
- Stopping antidepressants. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur. So stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, sometimes called discontinuation syndrome. Don't stop taking your medication without talking to your doctor, even if you're feeling better — you may have a relapse of OCD symptoms. Work with your doctor to gradually and safely decrease your dose.
Talk to your doctor about the risks and benefits of using specific medications.
Other treatment
Sometimes, psychotherapy and medications aren't effective enough to control OCD symptoms. In treatment-resistant cases, other options may be offered:
- Intensive outpatient and residential treatment programs. Comprehensive treatment programs that emphasize ERP therapy principles may be helpful for people with OCD who struggle with being able to function because of the severity of their symptoms. These programs typically last several weeks.
- Deep brain stimulation (DBS). DBS is approved by the FDA to treat OCD in adults age 18 years and older who don't respond to traditional treatment approaches. DBS involves implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that may help regulate abnormal impulses.
- Transcranial magnetic stimulation (TMS). The FDA approved a specific device (BrainsWay Deep Transcranial Magnetic Stimulation) to treat OCD in adults ages 22 to 68 years, when traditional treatment approaches have not been effective. TMS is a noninvasive procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms of OCD. During a TMS session, an electromagnetic coil is placed against your scalp near your forehead. The electromagnet delivers a magnetic pulse that stimulates nerve cells in your brain.
Talk with your doctor to make sure you understand all the pros and cons and possible health risks of DBS and TMS if you're considering one of these procedures.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Obsessive-compulsive disorder (OCD) and Learn More about Diseases

Spider bites

Infant reflux
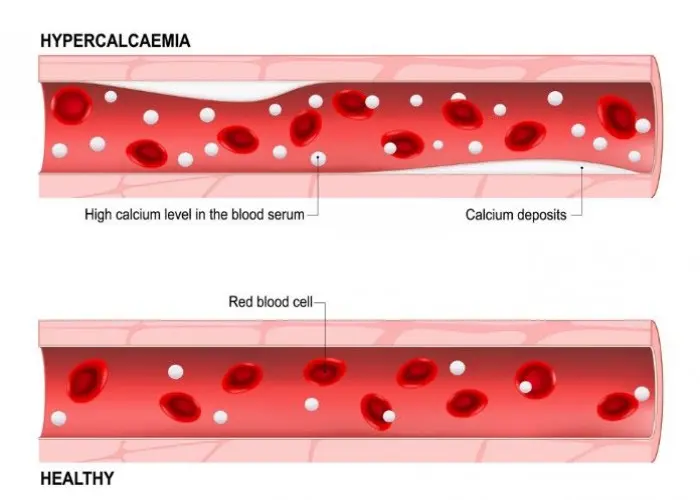
Hypercalcemia

Wrist pain
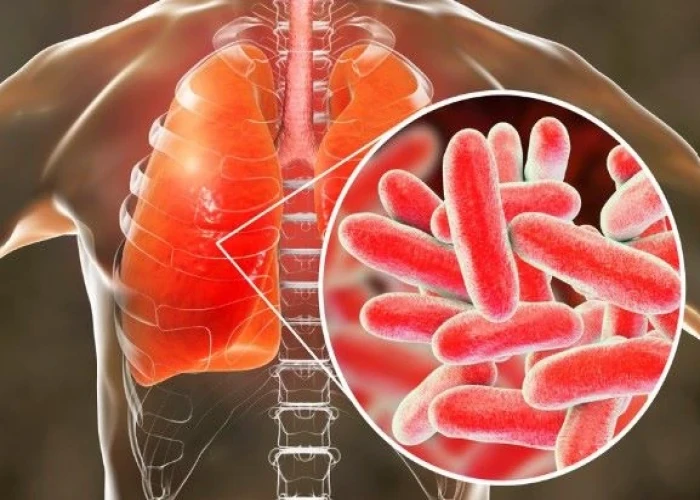
Legionnaires' disease

Schizotypal personality disorder

Small intestinal bacterial overgrowth (SIBO)
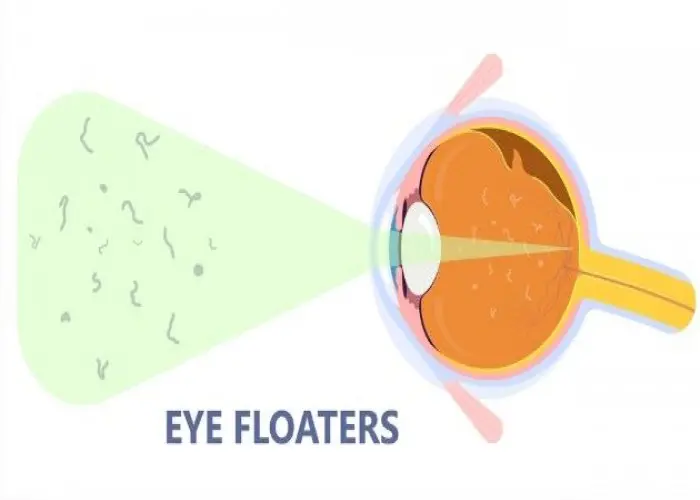
Eye floaters
obsessive-compulsive disorder, ocd, অবসেসিভ-বাধ্যতামূলক ব্যাধি, ওসিডি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
