Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
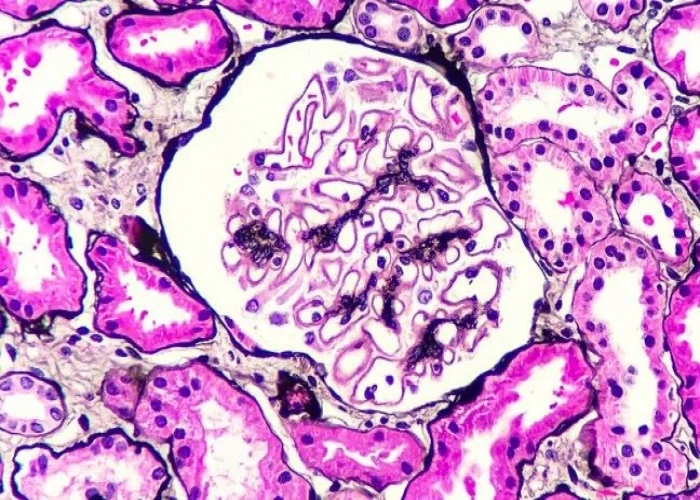
Membranous nephropathy

Membranous nephropathy is a type of kidney disease that affects the glomeruli, the small blood vessels in the kidneys that filter waste from the blood. It is characterized by the thickening of the glomerular basement membrane, which can impair the kidneys' ability to filter blood properly and cause proteinuria (the presence of protein in the urine).
The exact cause of membranous nephropathy is unknown, but it is thought to be an autoimmune disorder in which the immune system attacks the glomeruli. Certain infections, medications, and underlying medical conditions such as diabetes and lupus can also increase the risk of developing the condition.
Symptoms of membranous nephropathy may include:
- Proteinuria (the presence of protein in the urine)
- Edema (swelling) in the legs, ankles, or feet
- High blood pressure
- Fatigue
- Loss of appetite
- Weight gain
To diagnose membranous nephropathy, a healthcare provider may perform a physical exam and order blood and urine tests to evaluate kidney function and the presence of protein in the urine. A kidney biopsy may also be performed to confirm the diagnosis.
Treatment for membranous nephropathy typically involves controlling underlying medical conditions and managing symptoms. Medications such as ACE inhibitors and angiotensin receptor blockers (ARBs) may be prescribed to control high blood pressure and reduce proteinuria. Immunosuppressive medications such as corticosteroids, cyclosporine, or rituximab may also be recommended to suppress the immune system and reduce inflammation in the kidneys.
In severe cases of membranous nephropathy, dialysis or kidney transplant may be necessary. It is important to work closely with a healthcare provider to manage the condition and prevent complications.
Research Papers
Disease Signs and Symptoms
- Swollen leg
- The spinning sensation starts and stops spontaneously.
- Decreased protein in the blood, particularly albumin
- High blood pressure (hypertension)
- Blood in urine (hematuria)
- Excess protein or cloudy urine (proteinuria)
- High cholesterol
- Loss of appetite
- Fatigue (Tiredness)
- Rapid weight gain
- Episodes of vertigo occur without warning and usually last 20 minutes to several hours, but not more than 24 hours.
Disease Causes
Membranous nephropathy
Often, membranous nephropathy results from some type of autoimmune activity. Your body's immune system mistakes healthy tissue as foreign and attacks it with substances called autoantibodies. These autoantibodies target certain proteins located in the kidney's filtering systems (glomeruli). This is known as primary membranous nephropathy.
Sometimes membranous nephropathy is brought on by other causes. When this happens, it's called secondary membranous nephropathy. Causes may include:
- Autoimmune disease, such as lupus erythematosus
- Infection with hepatitis B, hepatitis C or syphilis
- Certain medications, such as gold salts and nonsteroidal anti-inflammatory drugs
- Solid cancerous tumors or blood cancers
Membranous nephropathy may also occur along with other kidney diseases, such as diabetic nephropathy and rapidly progressive (crescentic) glomerulonephritis.
Disease Prevents
Disease Treatments
Treatment of membranous nephropathy focuses on addressing the cause of your disease and relieving your symptoms. There is no certain cure.
However, up to three out of 10 people with membranous nephropathy have their symptoms completely disappear (remission) after five years without any treatment. About 25 to 40 percent have a partial remission.
In cases where membranous nephropathy is caused by a medication or another disease — such as cancer — stopping the medication or controlling the other disease usually improves the condition.
Low risk of advanced kidney disease
With membranous nephropathy, you're considered at low risk of developing advanced kidney disease in the next five years if:
- Your urine protein level remains less than 4 grams a day for six months
- Your blood creatinine level remains in the normal range for six months
If you're at low risk of advanced kidney disease, treatment of membranous nephropathy usually begins by taking the following steps:
- Take blood pressure medication. Doctors typically prescribe an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin II receptor blocker (ARB) to keep your blood pressure under control.
- Decrease swelling (edema). Water pills (diuretics) help remove sodium and water from your blood.
- Control cholesterol. Medications called statins are used to keep your cholesterol in check.
- Lower your risk for blood clots. People with membranous nephropathy are more likely to have deep vein thrombosis or pulmonary embolism. Doctors may prescribe blood-thinners, or anticoagulants, to prevent these dangerous events.
- Cut back on salt. Salt can increase urine protein levels. It also makes your body retain fluid. Check the salt content in foods, drinks and condiments.
Doctors generally prefer to avoid using strong drugs (which can cause significant side effects) early in the course of the disease, when there's a chance that the disease will improve on its own.
Moderate to high risk of advanced kidney disease
Your doctor may recommend more-intensive treatment as the amount of protein in your urine increases. The more protein you have in your urine (proteinuria), the greater the risk to your kidneys and well-being.
In the past, doctors have assessed risk based on the amount of protein in the urine over time:
- Moderate risk. Urine protein level stays between 4 and 8 grams a day and blood creatinine level is at normal or near normal for six months of observation. About half the people with these signs develop serious kidney disease over five years.
- High risk. Urine protein level is persistently greater than 8 grams a day for three months or kidney function is below normal or falls below normal during the observation period. About 3 out of 4 people with these signs are highly likely to develop serious kidney disease over 10 years.
A new approach for assessing risk allows doctors to evaluate antibody levels in the blood along with how much protein is in the urine. This approach also helps doctors determine how you'll respond to therapy.
If you have a moderate to high risk of advanced kidney disease, your doctor may talk to you about these treatments for membranous nephropathy:
- Steroids plus a chemotherapy drug. If your urine protein level keeps rising, your doctor may prescribe a corticosteroid medication with a chemotherapy drug to suppress your immune system. This can lower your urine protein levels and stop the progress toward kidney failure. However, immune suppressing medications don't help everyone. They can also have significant side effects. Some of the side effects of chemotherapy drugs — such as risk of cancer or infertility — may occur many years after taking the drug.
- Cyclosporine. If you don't want to take a chemotherapy drug or cannot tolerate it, cyclosporine (a calcineurin inhibitor drug) is an option.
- Rituximab (Rituxan). Rituximab has helped some people who have not improved with immunosuppressive therapy. Studies suggest it works at least as well as steroid therapy. The medication kills B cells in the immune system — the cells that produce substances, called antibodies, that damage the glomeruli. However, it's expensive and not generally covered by insurance.
Sometimes, the disease comes back after treatment ends. This has happened to people taking any kind of immune suppressants. In some cases, if the first round of treatment doesn't work or you have a relapse, you may benefit from a second round. Talk to your doctor about the best treatment plan for you.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Membranous nephropathy and Learn More about Diseases

Uveitis
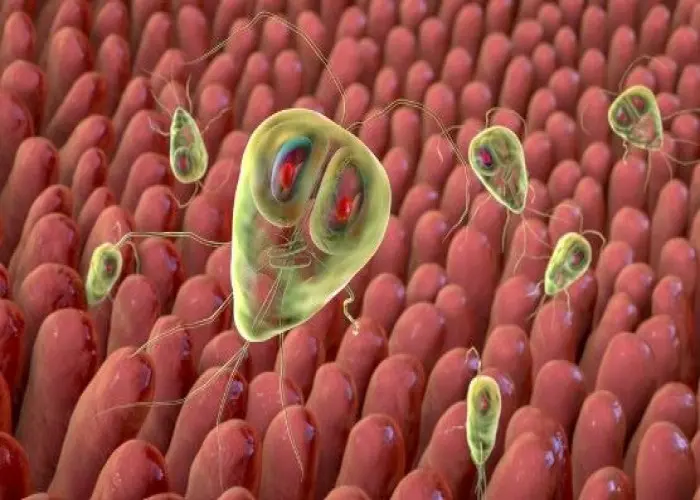
Giardia infection (Giardiasis)

Rectal cancer

Progeria

Gestational diabetes

Group B strep disease
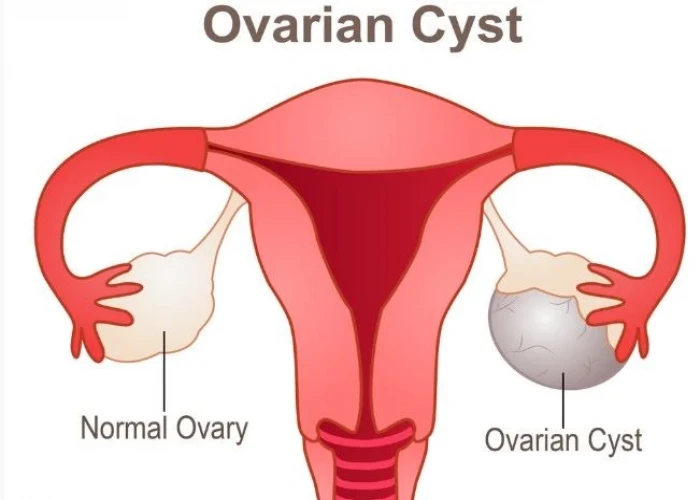
Ovarian cysts
Acute flaccid myelitis (AFM)
membranous nephropathy, ঝিল্লি নেফ্রোপ্যাথি
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.