 Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Interstitial cystitis

Interstitial cystitis (IC) is a chronic condition that causes inflammation of the bladder wall, resulting in pain, discomfort, and frequent urination. The cause of IC is not fully understood, but it is believed to be related to abnormalities in the protective lining of the bladder, which allows irritating substances in urine to penetrate the bladder wall and cause inflammation.
Symptoms of IC may include pain or discomfort in the bladder or pelvic area, a frequent need to urinate, urgency to urinate, and pain during sexual intercourse. These symptoms may vary in severity from person to person and may be intermittent or constant.
Diagnosis of IC may involve a comprehensive medical evaluation, including a physical examination, urinalysis, urine culture, and cystoscopy. Treatment for IC may include medications to reduce inflammation and alleviate pain, bladder training to help reduce frequency and urgency of urination, and dietary modifications such as avoiding certain foods and beverages that may irritate the bladder. In some cases, more invasive treatments such as bladder distension, nerve stimulation, or surgery may be recommended.
Living with IC may involve making lifestyle changes to manage symptoms, such as avoiding certain foods and beverages, reducing stress, and practicing good hygiene habits. It is important for individuals with IC to work closely with their healthcare provider to develop a treatment plan that addresses their specific needs and symptoms.
Research Papers
Disease Signs and Symptoms
- Anus pain
- Frequent urination
- Pain or discomfort while the bladder fills and relief after urinating.
- Symptoms severity is different for everyone, and some people may experience symptom-free periods.
- Shortness of breath at rest or aggravated by exertion
- Interstitial cystitis or painful bladder syndrome
Disease Causes
Interstitial cystitis
The exact cause of interstitial cystitis isn't known, but it's likely that many factors contribute. For instance, people with interstitial cystitis may also have a defect in the protective lining (epithelium) of the bladder. A leak in the epithelium may allow toxic substances in urine to irritate your bladder wall.
Other possible but unproven contributing factors include an autoimmune reaction, heredity, infection or allergy.
Disease Prevents
Disease Treatments
No simple treatment eliminates the signs and symptoms of interstitial cystitis, and no one treatment works for everyone. You may need to try various treatments or combinations of treatments before you find an approach that relieves your symptoms.
Physical therapy
Working with a physical therapist may relieve pelvic pain associated with muscle tenderness, restrictive connective tissue or muscle abnormalities in your pelvic floor.
Oral medications
Certain medicines that you take by mouth (oral medications) may improve signs and symptoms of interstitial cystitis:
- Nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve), to relieve pain.
- Tricyclic antidepressants, such as amitriptyline or imipramine (Tofranil), to help relax your bladder and block pain.
- Antihistamines, such as loratadine (Claritin, others), which may reduce urinary urgency and frequency and relieve other symptoms.
- Pentosan polysulfate sodium (Elmiron), which is approved by the Food and Drug Administration specifically for treating interstitial cystitis. How it works is unknown, but it may restore the inner surface of the bladder, which protects the bladder wall from substances in urine that could irritate it. It may take two to four months before you begin to feel pain relief and up to six months to experience a decrease in urinary frequency.
- Macular eye disease has been associated with use of this medication in some people. Before starting this treatment, you may need a comprehensive eye exam. You may also need additional eye exams to monitor for eye disease as you continue therapy.
Nerve stimulation
Nerve stimulation techniques include:
- Transcutaneous electrical nerve stimulation (TENS). With TENS, mild electrical pulses relieve pelvic pain and, in some cases, reduce urinary frequency. TENS may increase blood flow to the bladder. This may strengthen the muscles that help control the bladder or trigger the release of substances that block pain.
- Electrical wires placed on your lower back or just above your pubic area deliver electrical pulses — the length of time and frequency of therapy depends on what works best for you.
- Sacral nerve stimulation. Your sacral nerves are a primary link between the spinal cord and nerves in your bladder. Stimulating these nerves may reduce urinary urgency associated with interstitial cystitis.
- With sacral nerve stimulation, a thin wire placed near the sacral nerves sends electrical impulses to your bladder, similar to what a pacemaker does for your heart. If the procedure decreases your symptoms, you may have a permanent device surgically implanted. This procedure doesn't manage pain from interstitial cystitis, but may help to relieve some symptoms of urinary frequency and urgency.
Bladder distention
Some people notice a temporary improvement in symptoms after cystoscopy with bladder distention. Bladder distention is the stretching of the bladder with water. If you have long-term improvement, the procedure may be repeated.
Botulinum toxin A (Botox) may be injected into the bladder wall during bladder distention. But, this treatment option could lead to not being able to empty your bladder completely when you urinate. You may need to self-catheterize — be able to insert a tube into your own bladder to drain urine — after this treatment.
Medications instilled into the bladder
In bladder instillation, your provider places the prescription medication dimethyl sulfoxide (Rimso-50) into your bladder through a thin, flexible tube (catheter) inserted through the urethra.
The solution sometimes is mixed with other medications, such as a local anesthetic, and remains in your bladder for about 15 minutes. You urinate to expel the solution.
You might receive dimethyl sulfoxide — also called DMSO — treatment weekly for six to eight weeks, and then have maintenance treatments as needed — such as every couple of weeks, for up to one year.
Another approach to bladder instillation uses a solution containing the medications lidocaine, sodium bicarbonate, and either pentosan or heparin.
Surgery
Doctors rarely use surgery to treat interstitial cystitis because removing the bladder doesn't relieve pain and can lead to other complications.
People with severe pain or those whose bladders can hold only very small volumes of urine are possible candidates for surgery, but usually only after other treatments fail and symptoms affect quality of life. Surgical options include:
- Fulguration. This minimally invasive method involves insertion of instruments through the urethra to burn off ulcers that may be present with interstitial cystitis.
- Resection. This is another minimally invasive method that involves insertion of instruments through the urethra to cut around any ulcers.
- Bladder augmentation. In this procedure, a surgeon increases the capacity of your bladder by putting a patch of intestine on the bladder. However, this is performed only in very specific and rare instances. The procedure doesn't eliminate pain and some people need to empty their bladders with a catheter many times a day.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Interstitial cystitis and Learn More about Diseases

Psoriasis

Rocky Mountain spotted fever
Sjogren's syndrome
Ocular rosacea
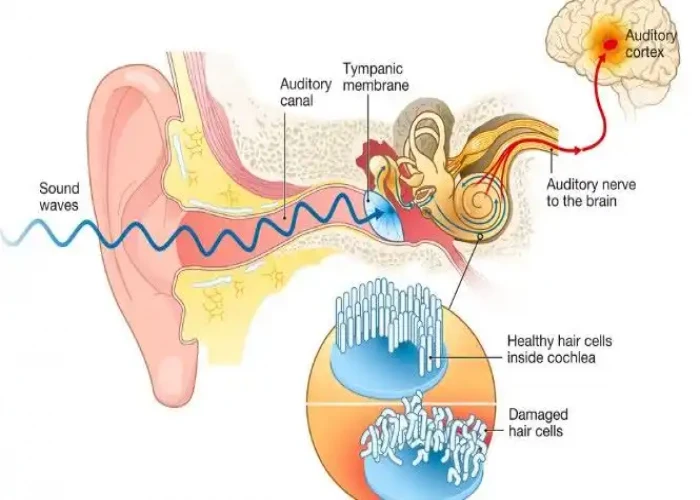
Tinnitus

Pinched nerve

MCAD deficiency

Monoclonal gammopathy of undetermined significance (MGUS)
interstitial cystitis, ইন্টারস্টিশিয়াল সিস্টাইতিস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.
