Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Hemolytic uremic syndrome (HUS)
Hemolytic uremic syndrome (HUS) is a serious medical condition that can cause acute kidney injury and other complications. It is most commonly caused by an infection with a particular strain of Escherichia coli (E. coli) bacteria, but can also be caused by other infections, medications, or genetic factors.
HUS is characterized by the destruction of red blood cells and the formation of blood clots in small blood vessels throughout the body, which can lead to kidney failure, anemia, and low platelet counts. Symptoms may include fatigue, abdominal pain, vomiting, diarrhea, and decreased urine output.
HUS is a medical emergency and requires immediate medical attention. Treatment typically involves hospitalization and supportive care, such as intravenous fluids, blood transfusions, and dialysis. Antibiotics are not recommended for the treatment of HUS, as they may actually worsen the condition in some cases.
Most people who develop HUS recover without long-term complications, but the condition can be fatal in some cases, particularly in children or older adults. Prevention measures, such as practicing good hygiene and food safety, can help reduce the risk of developing HUS.
If you or someone you know is experiencing symptoms of HUS, such as bloody diarrhea, abdominal pain, or decreased urine output, it is important to seek immediate medical attention.
Research Papers
Disease Signs and Symptoms
- Diarrhea
- High blood pressure (hypertension)
- Confusion (Hallucinations)
- Shortness of breath (dyspnea)
- Fever
- Nausea or vomiting
- Abdomen bloating
- Cramp
- Abdomen pain
- Unusual bleeding
Disease Causes
Hemolytic uremic syndrome (HUS)
The most common cause of HUS — particularly in children under the age of 5 — is infection with certain strains of E. coli bacteria. E. coli refers to a group of bacteria normally found in the intestines of healthy humans and animals. Most of the hundreds of types of E. coli are normal and harmless. But some strains of E. coli cause diarrhea.
Some of the E.coli strains that cause diarrhea also produce a toxin called Shiga toxin. These strains are called Shiga toxin-producing E. coli, or STEC. When you are infected with a strain of STEC, the Shiga toxin can enter your bloodstream and cause damage to your blood vessels, which may lead to HUS. But most people who are infected with E. coli, even the more dangerous strains, don't develop HUS.
Other causes of HUS can include:
- Other infections, such as infection with pneumococcal bacteria, human immunodeficiency virus (HIV) or influenza
- The use of certain medications, especially some of the medications used to treat cancer and some of the medications used to suppress the immune system of organ transplant recipients
- Rarely, HUS may occur as a complication of pregnancy or health conditions such as autoimmune disease or cancer
An uncommon type of HUS — known as atypical HUS — can be passed down genetically to children. People who have inherited the mutated gene that causes this form of HUS won't necessarily develop the condition. But the mutated gene might be activated after exposure to a trigger, such as an infection, the use of certain medications or a chronic health condition.
Disease Prevents
Hemolytic uremic syndrome (HUS)
Meat or produce contaminated with E. coli won't necessarily look, feel or smell bad. To protect against E. coli infection and other foodborne illnesses:
- Avoid unpasteurized milk, juice and cider.
- Wash hands well before eating and after using the restroom and changing diapers.
- Clean utensils and food surfaces often.
- Cook meat to an internal temperature of at least 160 degrees Fahrenheit.
- Defrost meat in the microwave or refrigerator.
- Keep raw foods separate from ready-to-eat foods. Don't place cooked meat on plates previously contaminated by raw meat.
- Store meat below produce in the refrigerator to reduce the risk of liquids such as blood dripping on produce.
- Avoid unclean swimming areas. Don't swim if you have diarrhea.
Disease Treatments
HUS requires treatment in the hospital. Lost fluids and electrolytes must be carefully replaced because the kidneys aren't removing fluids and waste as efficiently as normal.
Transfusions
In the hospital, you may need intravenous (IV) transfusions of red blood cells or platelets.
- Red blood cells can help reverse signs and symptoms of anemia — including chills, fatigue, shortness of breath, rapid heart rate, yellow skin and dark urine.
- Platelets can help your blood clot more normally if you're bleeding or bruising easily.
Medications
If you have lasting kidney damage from HUS, your doctor might recommend a medication to lower your blood pressure, to prevent or delay further kidney damage.
If you develop complications or have the form of HUS that's caused by a genetic mutation (atypical HUS), your doctor may recommend eculizumab (Soliris) to help prevent additional damage to your blood vessels.
Before taking eculizumab, you will need to receive or have already received a vaccination to prevent meningitis, a potential and serious side effect of the medicine.
Surgery and other procedures
Depending on your symptoms, the cause of your HUS and whether you have any complications, your doctor may recommend other treatments, including:
- Kidney dialysis. Sometimes dialysis is needed to filter waste and excess fluid from the blood. Dialysis is usually a temporary treatment until the kidneys begin functioning adequately again. But if you have significant kidney damage, you might need long-term dialysis.
- Plasma exchange. Plasma is the fluid part of blood that supports the circulation of blood cells and platelets. Sometimes a machine is used to clear the blood of its own plasma and replace it with fresh or frozen donor plasma.
- Kidney transplant. Some people who have severe kidney damage from HUS eventually will need a kidney transplant.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Hemolytic uremic syndrome (HUS) and Learn More about Diseases

Polio

Male hypogonadism

Cyclic vomiting syndrome
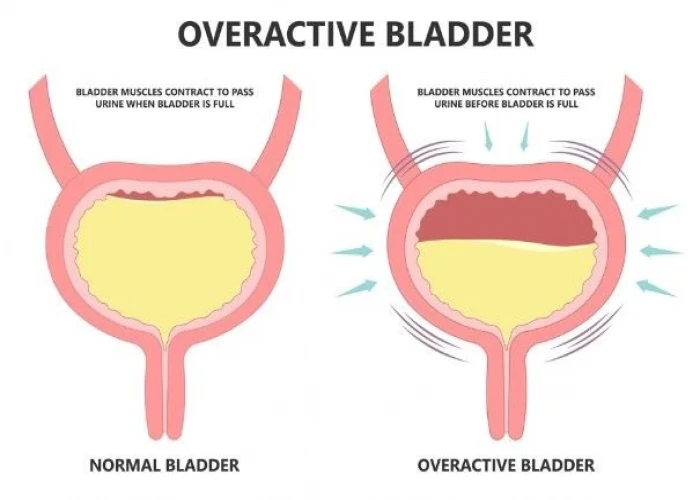
Overactive bladder
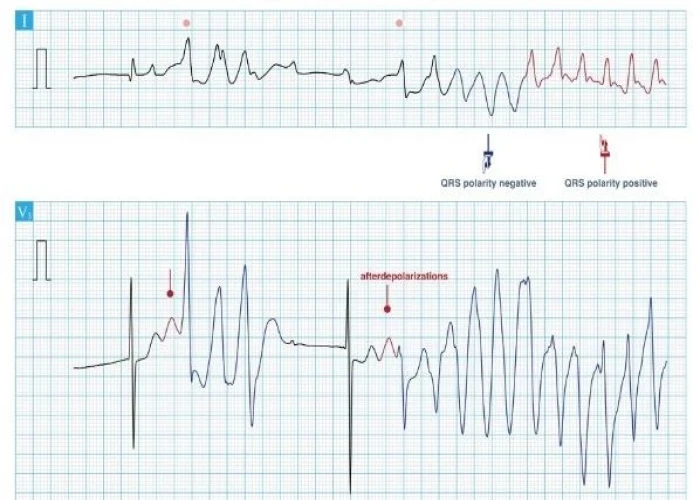
Long QT syndrome

Meningioma
Chronic sinusitis

Mitral valve disease
hemolytic uremic syndrome, hus, হিমোলিটিক ইউরেমিক সিনড্রোম, এইচইউএস
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.