Welcome
Welcome
“May all be happy, may all be healed, may all be at peace and may no one ever suffer."
Coronavirus disease 2019 (COVID-19)

Coronavirus disease 2019 (COVID-19) is an infectious respiratory illness caused by the novel coronavirus SARS-CoV-2. The disease was first identified in December 2019 in Wuhan, China and has since become a global pandemic, affecting millions of people worldwide.
COVID-19 spreads primarily through respiratory droplets when an infected person talks, coughs, or sneezes. It can also spread by touching surfaces contaminated with the virus and then touching one's mouth, nose, or eyes. Symptoms of COVID-19 can range from mild to severe and include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
COVID-19 can be diagnosed through laboratory tests, such as a polymerase chain reaction (PCR) test or a rapid antigen test. Treatment for COVID-19 typically involves supportive care, such as rest, hydration, and over-the-counter pain relievers. Severe cases may require hospitalization and more intensive treatments, such as oxygen therapy or mechanical ventilation.
Prevention of COVID-19 involves following public health guidelines, such as wearing masks, practicing physical distancing, avoiding large gatherings, washing hands frequently, and getting vaccinated. Vaccines have been shown to be highly effective at preventing severe illness, hospitalization, and death from COVID-19.
COVID-19 has had a significant impact on individuals, communities, and societies around the world. As the pandemic continues, it is important to stay informed about the latest developments, follow public health guidelines, and seek medical care if experiencing symptoms of COVID-19.
Research Papers
Disease Signs and Symptoms
- Fever
- Skin rash
- Diarrhea
- Nausea or vomiting
- Pink eye (conjunctivitis)
- Chest pain
- Headaches
- Runny nose
- Throat pain
- Fever and chills
- Muscle pain
- Difficulty breathing (dyspnea)
- Shortness of breath (dyspnea)
- Fatigue (Tiredness)
- Dry cough
- Cough
Disease Causes
Coronavirus disease 2019 (COVID-19)
Infection with severe acute respiratory syndrome coronavirus 2, or SARS-CoV-2, causes coronavirus disease 2019 (COVID-19).
The virus that causes COVID-19 spreads easily among people. Data has shown that the COVID-19 virus spreads mainly from person to person among those in close contact (within about 6 feet, or 2 meters). The virus spreads by respiratory droplets released when someone with the virus coughs, sneezes, breathes, sings or talks. These droplets can be inhaled or land in the mouth, nose or eyes of a person nearby.
Sometimes the COVID-19 virus can spread when a person is exposed to very small droplets or aerosols that stay in the air for several minutes or hours — called airborne transmission.
The virus can also spread if you touch a surface with the virus on it and then touch your mouth, nose or eyes. But the risk is low.
The COVID-19 virus can spread from someone who is infected but has no symptoms. This is called asymptomatic transmission. The COVID-19 virus can also spread from someone who is infected but hasn't developed symptoms yet. This is called presymptomatic transmission.
It's possible to get COVID-19 twice or more, but this is uncommon.
When a virus has one or more new mutations it’s called a variant of the original virus. Currently, the CDC has identified two variants of the virus that causes COVID-19 as variants of concern. These include the delta (B.1.617.2) variant and the omicron (B.1.1.529) variant. The delta variant is more contagious than earlier variants and might cause more severe disease. The omicron variant might spread more easily than other variants, including delta. But it’s not yet clear if omicron causes more severe disease.
Disease Prevents
Coronavirus disease 2019 (COVID-19)
The U.S. Food and Drug Administration (FDA) has given emergency use authorization to some COVID-19 vaccines in the United States. The FDA has approved the Pfizer-BioNTech COVID-19 vaccine, now called Comirnaty, to prevent COVID-19 in people age 16 and older. The FDA has given emergency use authorization to Pfizer-BioNTech COVID-19 vaccines for ages 5 through 15. The FDA has approved the Moderna vaccine, now called Spikevax, to prevent COVID-19 in people age 18 and older.
A vaccine can prevent you from getting the COVID-19 virus or prevent you from becoming seriously ill if you get the COVID-19 virus. In addition, COVID-19 vaccination might offer better protection than getting sick with COVID-19. A recent study showed that unvaccinated people who already had COVID-19 are more than twice as likely as fully vaccinated people to get reinfected with COVID-19.
After getting vaccinated, you can more safely return to many activities you may not have been able to do because of the pandemic. However, if you are in an area with a high number of people with COVID-19 in the hospital and new COVID-19 cases, the CDC recommends wearing a mask indoors in public. You're considered fully vaccinated two weeks after you get a second dose of an mRNA COVID-19 vaccine or two weeks after you get a single dose of the Janssen/Johnson & Johnson COVID-19 vaccine. You are considered up to date with your vaccines if you have gotten all recommended COVID-19 vaccines, including booster doses, when you become eligible.
An additional primary dose of a COVID-19 vaccine is recommended for people who are vaccinated and might not have had a strong enough immune response.
In contrast, a booster dose is recommended for people who are vaccinated and whose immune response weakened over time. Research suggests that getting a booster dose can decrease your risk of infection and severe illness with COVID-19.
People who have a moderately or severely weakened immune system should get an additional primary shot and a booster shot.
The CDC recommends additional doses and booster doses of COVID-19 vaccines in specific instances:
- Additional dose. The CDC recommends a third dose of an mRNA COVID-19 vaccine for some people with weakened immune systems, such as those who have had an organ transplant. People with weakened immune systems might not develop enough immunity after vaccination with two doses of an mRNA COVID-19 vaccine. An additional dose might improve their protection against COVID-19.
- The third dose should be given at least 28 days after a second dose of an mRNA COVID-19 vaccine. The additional dose should be the same brand as the other two mRNA COVID-19 vaccine doses you were given. If the brand given isn't known, either brand of mRNA COVID-19 vaccine can be given as a third dose.
- Booster dose. If you are age 12 or older, have been given both doses of the Pfizer-BioNTech COVID-19 vaccine and it’s been at least 5 months, you should get a single booster dose. Teens ages 12 to 17 should only get the Pfizer-BioNTech COVID-19 vaccine booster. For people age 18 or older, the Pfizer-BioNTech or Moderna COVID-19 vaccine boosters are preferred in most situations.
- If you are age 18 or older, have been given both doses of the Moderna COVID-19 vaccine and it’s been at least 5 months, you should get a single booster dose. The Pfizer-BioNTech or Moderna COVID-19 vaccine boosters are preferred in most situations.
- If you are age 18 or older, have been given one dose of the Janssen/Johnson & Johnson COVID-19 vaccine and it’s been at least 2 months, you should get a single booster dose. The Pfizer-BioNTech or Moderna COVID-19 vaccine boosters are preferred in most situations.
- Pregnant women may also receive a COVID-19 booster shot.
The FDA has also authorized the monoclonal antibodies tixagevimab and cilgavimab (Evusheld) to prevent COVID-19 in some people with weakened immune systems or a history of severe reactions to a COVID-19 vaccine.
There are many steps you can take to reduce your risk of infection from the COVID-19 virus and reduce the risk of spreading it to others. WHO and CDC recommend following these precautions:
- Get vaccinated. COVID-19 vaccines reduce the risk of getting and spreading COVID-19.
- Avoid close contact (within about 6 feet, or 2 meters) with anyone who is sick or has symptoms.
- Keep distance between yourself and others (within about 6 feet, or 2 meters) when you're in indoor public spaces if you're not fully vaccinated. This is especially important if you have a higher risk of serious illness. Keep in mind some people may have COVID-19 and spread it to others, even if they don't have symptoms or don't know they have COVID-19.
- Avoid crowds and indoor places that have poor air flow (ventilation).
- Wash your hands often with soap and water for at least 20 seconds, or use an alcohol-based hand sanitizer that contains at least 60% alcohol.
- Wear a face mask in indoor public spaces if you're in an area with a high number of people with COVID-19 in the hospital and new COVID-19 cases, whether or not you're vaccinated. The CDC recommends wearing the most protective mask possible that you'll wear regularly, fits well and is comfortable.
- Cover your mouth and nose with your elbow or a tissue when you cough or sneeze. Throw away the used tissue. Wash your hands right away.
- Avoid touching your eyes, nose and mouth.
- Avoid sharing dishes, glasses, towels, bedding and other household items if you're sick.
- Clean and disinfect high-touch surfaces, such as doorknobs, light switches, electronics and counters, regularly.
- Stay home from work, school and public areas and stay home in isolation if you're sick, unless you're going to get medical care. Avoid public transportation, taxis and ride-hailing services if you're sick.
If you have a chronic medical condition and may have a higher risk of serious illness, check with your doctor about other ways to protect yourself.
Disease Treatments
Currently, only one medication has been approved to treat COVID-19. No cure is available for COVID-19. Antibiotics aren't effective against viral infections such as COVID-19. Researchers are testing a variety of possible treatments.
The FDA has approved the antiviral drug remdesivir (Veklury) to treat COVID-19 in hospitalized adults and children who are age 12 and older in the hospital. Remdesivir may be prescribed for people who are hospitalized with COVID-19 and need supplemental oxygen or have a higher risk of serious illness. It's given through a needle in the skin (intravenously).
The FDA has authorized a drug called Paxlovid that includes nirmatrelvir – a drug that blocks the activity of a specific enzyme needed for the virus that causes COVID-19 to replicate – and an antiviral drug called ritonavir that helps slow the breakdown of nirmatrelvir. Paxlovid is authorized to treat mild to moderate COVID-19 in people age 12 and older who are at higher risk of serious illness. The medications are taken by mouth as pills.
The FDA has authorized another drug called molnupiravir to treat mild to moderate COVID-19 in adults who are at higher risk of serious illness and who aren't able to take other treatment options. The medication is taken by mouth as a pill.
The FDA has authorized the rheumatoid arthritis drug baricitinib (Olumiant) to treat COVID-19 in some cases. Baricitinib is a pill that seems to work against COVID-19 by reducing inflammation and having antiviral activity. Baricitinib may be used in people who are hospitalized with COVID-19 who are on mechanical ventilators or need supplemental oxygen.
Monoclonal antibody medications include sotrovimab; bebtelovimab; a combination of bamlanivimab and etesevimab; and a combination of casirivimab and imdevimab. Some monoclonal antibodies, including bamlanivimab and etesevimab and casirivimab and imdevimab, aren't effective against COVID-19 caused by the omicron variant. However, sotrovimab and bebtelovimab can be used to treat COVID-19 caused by the omicron variant.
These drugs are used to treat mild to moderate COVID-19 in people who have a higher risk of developing serious illness due to COVID-19. Treatment involves a single infusion given by a needle in the arm (intravenously) in an outpatient setting. To be most effective, these medications need to be given soon after COVID-19 symptoms start and prior to hospitalization.
The U.S. National Institutes of Health has recommended the corticosteroid dexamethasone for people hospitalized with severe COVID-19 who are on supplemental oxygen or need mechanical ventilation. Other corticosteroids, such as prednisone, methylprednisolone or hydrocortisone, may be used if dexamethasone isn't available.
In some cases, the drugs remdesivir, tocilizumab or baricitinib may be given with dexamethasone in hospitalized people who are on mechanical ventilation or need supplemental oxygen.
The FDA has also authorized convalescent plasma therapy with high antibody levels to treat COVID-19. Convalescent plasma is blood donated by people who've recovered from COVID-19. Convalescent plasma with high antibodies may be used to treat some hospitalized people ill with COVID-19 who are either early in their illness or who have weakened immune systems.
Many people with COVID-19 may have mild illness and can be treated with supportive care. Supportive care is aimed at relieving symptoms and may include:
- Pain relievers (ibuprofen or acetaminophen)
- Cough syrup or medication
- Rest
- Fluid intake
There is no evidence that ibuprofen or other nonsteroidal anti-inflammatory drugs (NSAIDs) need to be avoided.
If you have mild symptoms, your health care provider will likely recommend that you recover at home. You may be given special instructions to monitor your symptoms and to avoid spreading the illness to others. You'll likely be asked to isolate yourself as much as possible from family and pets while you're sick, wear a mask when you're around people and pets, and use a separate bedroom and bathroom.
Your health care provider will likely recommend that you stay in home isolation for a period of time except to get medical care. Your health care provider will likely follow up with you regularly. Follow guidelines from your health care provider and local health department about when you can end home isolation.
If you're very ill, you may need to be treated in the hospital.
Disease Diagnoses
Disease Allopathic Generics
Disease Ayurvedic Generics
Disease Homeopathic Generics
Disease yoga
Coronavirus disease 2019 (COVID-19) and Learn More about Diseases
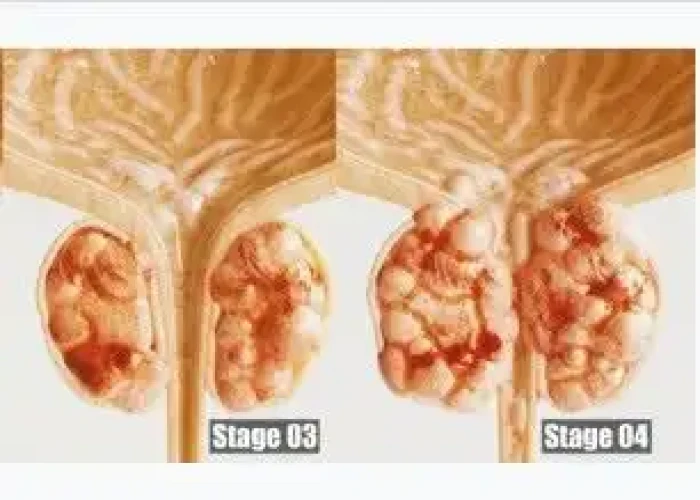
Stage 4 prostate cancer

Prader-Willi syndrome

Encopresis

Hypereosinophilic syndrome

Bed-wetting

Raynaud's disease

Mononucleosis
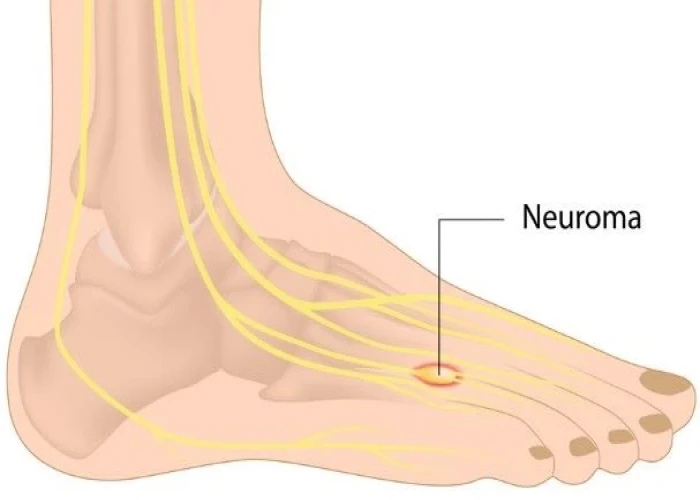
Morton's neuroma
COVID 2019, Coronavirus disease 2019, Corona, কোভিড-১৯, করোনাভাইরাস রোগ ২০১৯, করোনা
To be happy, beautiful, healthy, wealthy, hale and long-lived stay with DM3S.